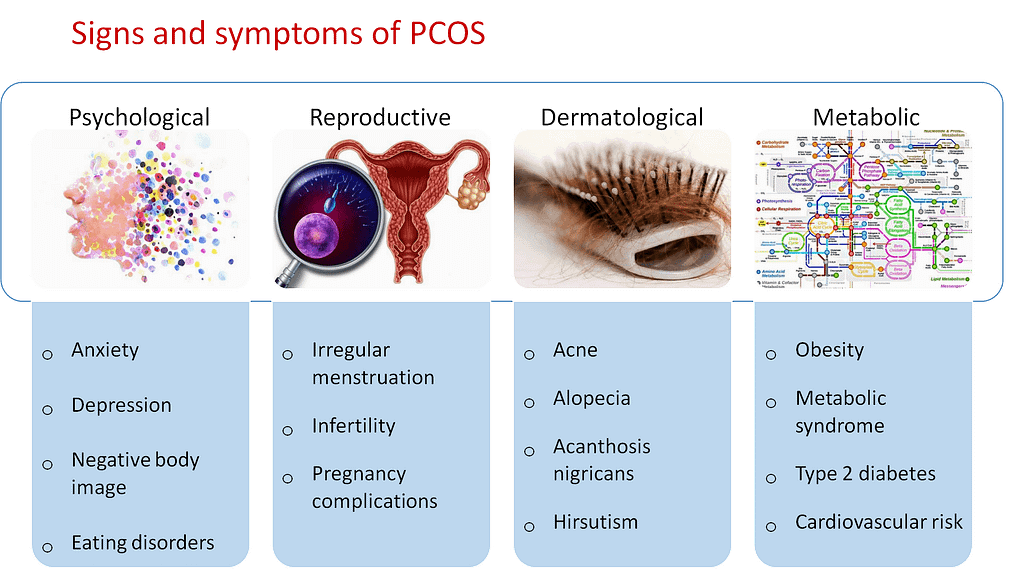
PCOS stands for Polycystic Ovary Syndrome. PCOS is most common endocrinopathy affecting reproductive aged women .It is heterogenous disorder defined by combination of signs and symptoms of Androgen excess .
PCOS is characterized by a combination of symptoms related to hormonal imbalances, menstrual irregularities, and the presence of multiple small cysts on the ovaries. The exact cause of PCOS is not fully understood, but it is believed to involve a combination of genetic and environmental factors.
Common symptoms of PCOS include irregular or absent menstrual periods, heavy or prolonged menstrual bleeding, excess hair growth (hirsutism), acne, weight gain or difficulty losing weight, and fertility problems. Women with PCOS may also experience insulin resistance, which can lead to high blood sugar levels and an increased risk of developing type 2 diabetes.
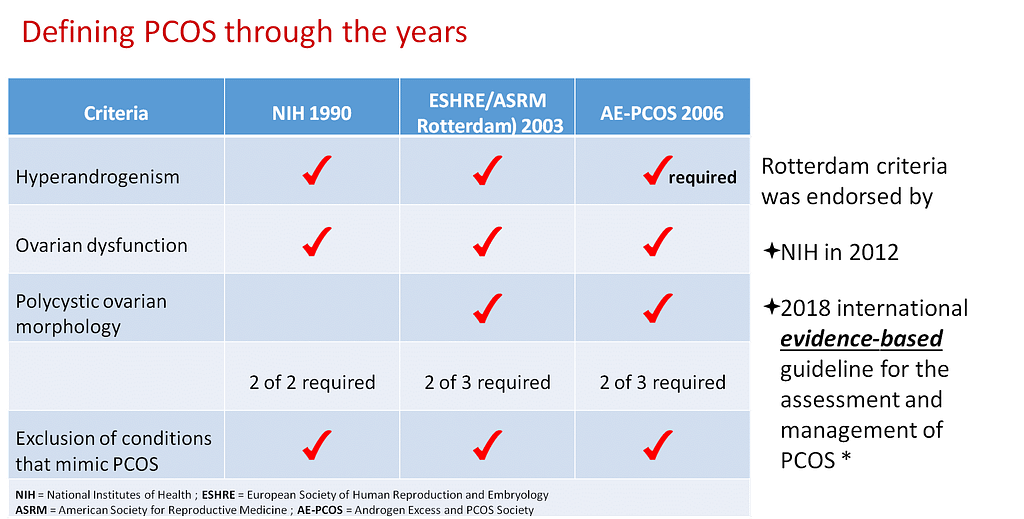
The Rotterdam criteria
One of the widely used diagnostic guidelines for PCOS and provide a broader definition compared to previous criteria.
According to the Rotterdam criteria, a diagnosis of PCOS can be made if two out of three criteria are met:
- Presence of irregular or absent menstrual cycles: This refers to the lack of regular ovulation, resulting in irregular periods or anovulatory cycles.
- Clinical or biochemical signs of hyperandrogenism: This includes the presence of excess androgen hormones (Testosterone,DHEAS,Free testosterone) in the body, which can manifest as hirsutism (excessive hair growth on the face, chest, or back), acne, or hyperandrogenemia (biochemical evidence of androgen excess).
- Ultrasonographic evidence of polycystic ovaries: This involves the presence of multiple small cysts on the ovaries, typically seen during an ultrasound examination. These cysts are often described as “string of pearls” appearance due to the clustering of follicles.
The European Society of Human Reproduction and Embryology (ESHRE) did release a revised definition of polycystic ovary syndrome (PCOS) in 2018. The ESHRE/ASRM Consensus on PCOS was published jointly by the European Society of Human Reproduction and Embryology (ESHRE) and the American Society for Reproductive Medicine (ASRM).
According to the 2018 ESHRE/ASRM Consensus on PCOS, the diagnosis of PCOS should be based on the presence of two out of three criteria, which are as follows:
- Oligo- or anovulation: This refers to irregular or absent menstrual cycles, indicating a lack of ovulation or infrequent ovulation.
- Clinical and/or biochemical signs of hyperandrogenism: This involves the presence of excess male hormones (androgens) in the body, which can manifest as hirsutism, acne, or hyperandrogenemia (biochemical evidence of androgen excess)
- Polycystic ovaries on ultrasound: This refers to the presence of multiple small cysts (follicles) on the ovaries, typically seen during an ultrasound examination. The criteria specify the presence of 12 or more follicles measuring 2-9 mm in diameter or an ovarian volume greater than 10 cm³.
- Exclusion of related disorders
It’s important to note that other potential causes of menstrual irregularities , hyperandrogenism, and ovarian cysts should be ruled out before making a diagnosis of PCOS.
The 2018 ESHRE/ASRM Consensus on PCOS also emphasized the need to consider the individual’s specific reproductive and metabolic characteristics when managing and treating PCOS.
Laboratory assesment of PCOS ESHRE 2018
For diagnosis and management of PCOS , Laboratory assesment is important following are the heading all in context of ESHRE 2018 RECOMMENDATION
1.Diagnosis of biochemical hyperandrogenism
2.Role of AMH
3.Evaluation of insulin resistance,gestational diabetes
4.cardiovascular risk in PCOS
Diagnosis of biochemical hyperandrogenism
Hyperandrogenism is the main criterion in the diagnostic work-up of polycystic ovary syndrome (PCOS). According to the current criteria, it can be indistinctly defined by either hirsutism and/or excess of blood testosterone
Assesment of biochemical hyperandogenism is particularly important when signs of hirsutism are unclear
Biochemical hyperandrogenism evaluation involves assessing the levels of androgen hormones in the blood to determine if there is an excess of androgens
It is recommended to calculate Free testosterone,free androgen index or calculated bioavailable testosterone
Androgen excess can be tested by measuring total and free testosterone levels or a free androgen index
An elevated free testosterone level is a sensitive indicator of androgen excess
- Most laboratories will offer a ‘free androgen index’(FAI)
- (FAI) which requires the measurement of SHBG and total testosterone and applying these in the formula:
- FAI = total testosterone/ SHBG x 100
- This effectively corrects for changes in SHBG but it does not take into account changes in the albumin‐bound

Most circulating testosterone is tightly bound to sex hormone-binding globulin (SHBG) or weakly bound to albumin.
- Factors that affect SHBG or albumin concentrations, such
as hyperthyroidism and posture, therefore result in changes in the bioavailable fraction of testosterone. The protein isoform and glycosylation status of SHBG also potentially impacts bioavailable testosterone by affecting the
dissociation constant (KD) between testosterone and this binding protein.- The free and albumin-bound forms comprise about 35% of total testosterone and are believed to be biologically
active.
- The free and albumin-bound forms comprise about 35% of total testosterone and are believed to be biologically
Testosterone estimation
- Isotope dilution mass spectrometry (MS) is the reference method for total and free testosterone measurement, but most labs rely on direct chemiluminescent immunoassays that displace bound forms of testosterone from SHBG and albumin. .
- Other methods used in clinical labs include liquid chromatography-tandem MS (LC-MS/MS) and gas chromatography MS. Both MS-based assays and immunoassays face the challenges of standardization across platforms and appropriate reference intervals partitioned for gender and age groups
AMH as pcos biomarker
- PCOS is also marked by arrested ovarian follicular development; women with this condition typically have an unusually high number of immature follicles detected by ultrasound.
- These immature follicles are precisely the ones that secrete AMH, making AMH an excellent surrogate marker for the antral follicle count, which is used to define the polycystic ovary element of the Rotterdam criteria
▪Current guidelines do not recommend AMH as an alternative to ultrasound
•May change with improved assay standardization and established cut off levels
FSH/LH ratio
Normally, FSH levels are higher than LH during the early follicular phase of the menstrual cycle, but in PCOS, LH levels can be elevated and the FSH/LH ratio may be lower than expected.
In polycystic ovary syndrome (PCOS), the follicle-stimulating hormone (FSH) to luteinizing hormone (LH) ratio is often altered compared to the typical hormonal balance seen in individuals without PCOS. However, it’s important to note that the FSH/LH ratio is not a diagnostic criteria for PCOS. PCOS is typically diagnosed based on a combination of symptoms, such as irregular menstrual cycles, excess androgen levels, and the presence of polycystic ovaries on ultrasound.
Investigations for glucose intolerance in PCOS
Prevalence of impaired glucose tolerance and type 2 diabetes mellitus is high in women with polycystic ovarian syndrome (PCOS) particularly those who have a body mass index (BMI) greater than 30 kg/m2 and have a strong family history of type 2 diabetes, or are older than 40 years—a 75-g oral glucose-tolerance test (OGTT) should be performed.
A 75-g oral glucose-tolerance test (OGTT) should be offered in all women with pcos preconception when planning pregnancy or seeking fertility treatment.Women diagnosed with prepregnancy PCOS should be screened for gestational diabetes before 20 weeks of gestation
A 2-hour postload glucose values
less than 140 mg/dL- indicates normal glucose tolerance
a value of 140-199 mg/dL – indicates impaired glucose tolerance
value of 200 mg/dL or higher- indicates diabetes mellitus
Cardiovascular risk assesment in PCOS
Insulin resistance dyslipidaemia and inflammatory markers (Hscrp) may help identify adolescent girls with PCOS who are at the highest risk of developing the metabolic syndrome .Lipid profile, HSCRP should be monitored to estimate the overall cardiovascular risk .
Differential diagnosis of PCOS
Non congenital adrenal hyperplasia
cushing syndrome
Thyroid dysfunction
Androgen secreting tumour
Adrenal hyperfunction
Hyperprolactinemia
ovarian tumours
