Pleural fluid analysis aids in identifying the origin of pleural effusion, distinguishing between bacterial, tuberculosis, and viral infections, and facilitating the diagnosis and staging of malignancies. This examination serves as a crucial diagnostic tool for determining the specific underlying cause and guiding appropriate treatment strategies for pleural effusions.
Clinical significance: Pleural fluid analysis is a test that examines a sample of fluid that has collected in the pleural space which when increased abnormally is called as pleural effusion
There are two main types of pleural effusion:
Transudate, which happens when there is an imbalance of pressure in certain blood vessels. Transudate pleural effusion is most often caused by heart failure or cirrhosis .
Exudate, which happens when there is an injury or inflammation of the pleura. Exudate pleural effusion has many causes. These include infections such as pneumonia , cancer , renal disease , and autoimmune diseases
| observation | Transudate | Exudate |
| Appearance | usually clear | cloudy |
| Fluid:serum protein ratio | < 0.5 | >0.5 |
| Fluid:serum Lactate Dehydrogenase ratio | < 0.60 | >0.60 |
WBC count | < 1000/µL | >1000/µL |
Pleural fluid cholesterol | < 45 mg/dL | >45mg/dL |
Pleural fluid:serum cholesterol ratio | < 0.30 | >0.30 |
Specimen collection: should be collected in tubes containing anticoagulants, such as EDTA( lavender top) or heparin
(green top), in order to avoid clotting and cell clumping, which may give inaccurate cell counts and differentials.
If microbiological analysis is indicated, inoculation of 2 to 5 mL pleural fluid into aerobic and anaerobic blood culture bottles, in addition to sending samples in a sterile tube for Gram stain.
TEST PROCEDURE
Investigation of fluid consists of:
Physical examination :
The normal appearance of a sample of pleural fluid is usually light yellow and clear. Abnormal results may give clues to the conditions or diseases present and may include:
1) Milky appearance may point to lymphatic system involvement.
2) Reddish pleural fluid may indicate the presence of blood.
3) Cloudy thick pleural fluid may indicate the presence of microorganisms and/or white blood cells.
4)Cobweb formation in tuberculosis.
Divide the sample into 2 parts. One for chemical analysis and another for smear examination.
Chemical examination: Includes the estimation of total proteins and glucose ,ADA, triglycerides ,enzymes like amylase if clinically indicated:
1) Glucose—typically about the same as blood glucose levels. May
be lower with infection and rheumatoid arthritis.
2) Lactate levels can increase with infectious pleuritis, either
bacterial or tuberculosis.
3) Amylase levels may increase with pancreatitis, oesophageal rupture, or malignancy.
4) Triglyceride levels may be increased with lymphatic systeminvolvement.
5)ADA adenosine deaminase raised in tubercular effusion
MICROSCOPIC EXAMINATION:
Includes the leukocyte count and red blood cell count of the uncentrifuge specimen. In addition; the sediment of the centrifuged specimen is taken for the study of the stained smear, for the direct examination of abnormal cells and differential count.
I. Total Cell Count: The WBCs and RBCs in the sample are counted.
Increased WBCs may be seen with infections and other causes of
pleuritis. Increased RBCs may suggest trauma, malignancy, or pulmonary
infarction.
Procedure for Estimation of Total Leukocyte Count/RBC Count:
1) Gently mix the specimen.
2) Add 20 µl of CSF diluting fluid in the labelled tubes.
4) To the tubes add 380 µl of well-mixed specimen.
5) Mix well and charge both sides of two Neubauer chambers.
6) Let it stand for 5 minutes and then observe under high power
objective.
7) Each chamber is observed by two different pathologists.
8) Count the number of WBC’s& RBC’s in four WBC squares (take a mean of both sides)
9) Calculate as follows:
WBC/RBC count/cmm= (Number of cells counted/4) x 10
10)If difference between the counts of two pathologists is found
up to 5%, the mean value is reported.
11)If difference between two count is >5%, the above procedure
needs to be repeated by another technician.
12)In cases where RBC’s interfere in counting of WBC’s, 380 µl of
WBC diluting fluid is added to 20µl of sample. Mix well and
keep for 10-15 mins. Charge the chamber and count 4 WBC
squares.
13)Calculate as follows:
WBC count/cmm= (Number of cells counted/4) x 200
For Chemical analysis:
1) Centrifuge the specimen at 2500 rpm for 10 minutes.
2) Transfer the supernatant on another tube for chemical analysis.
II. Differential Leukocyte Count:
For smear examination for estimation of differential count:
1) Process the sample using cytospin at 1000 rpm for 10 mins
2) Smear formed on slide are left to dry
3) Stain the slide with Leishman stain and observe under oil immersion
Interpretation:
An increased number of neutrophils may be seen with bacterial infections.
An increased number of lymphocytes may be seen with tuberculosis &
other chronic conditions.
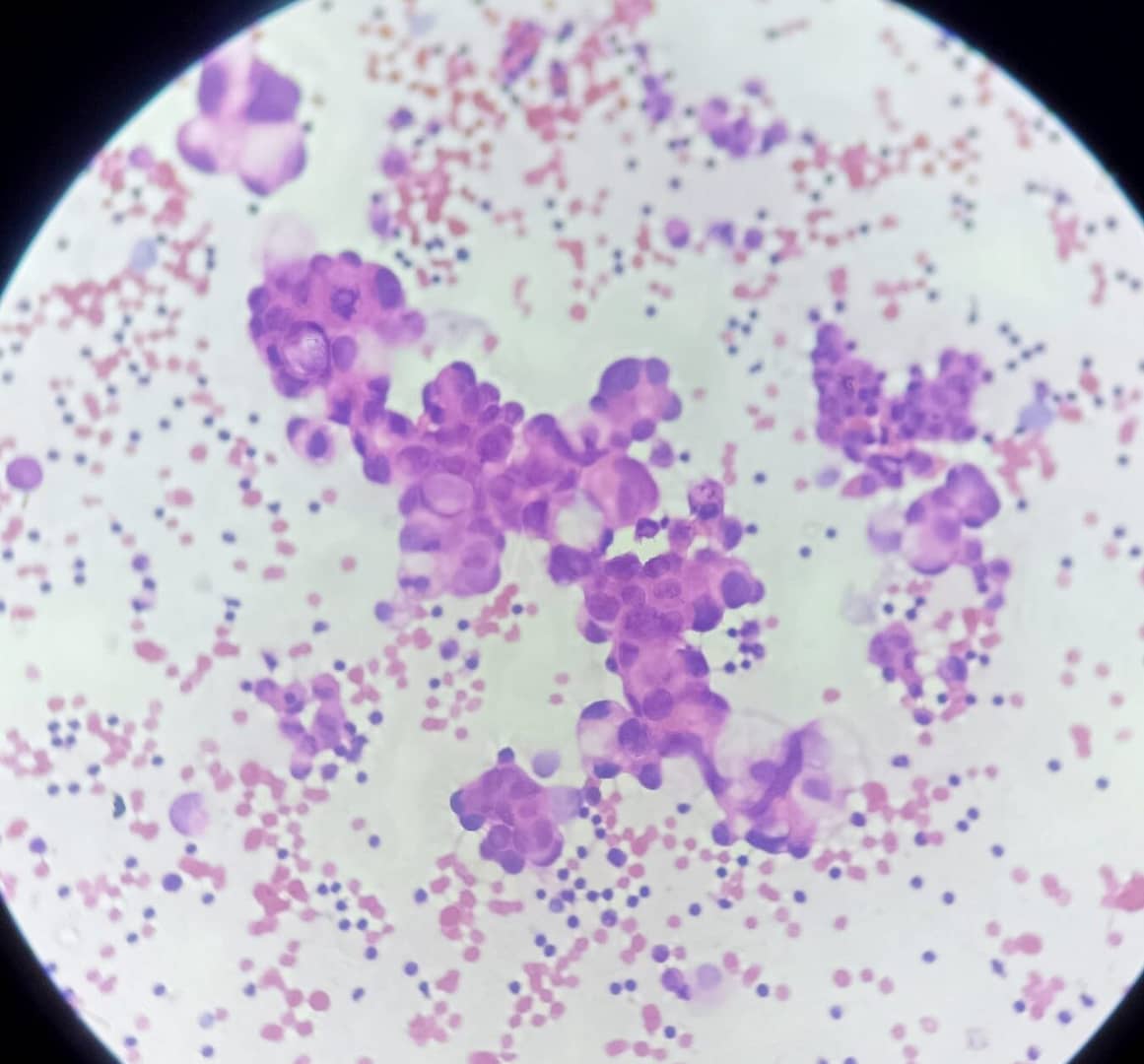
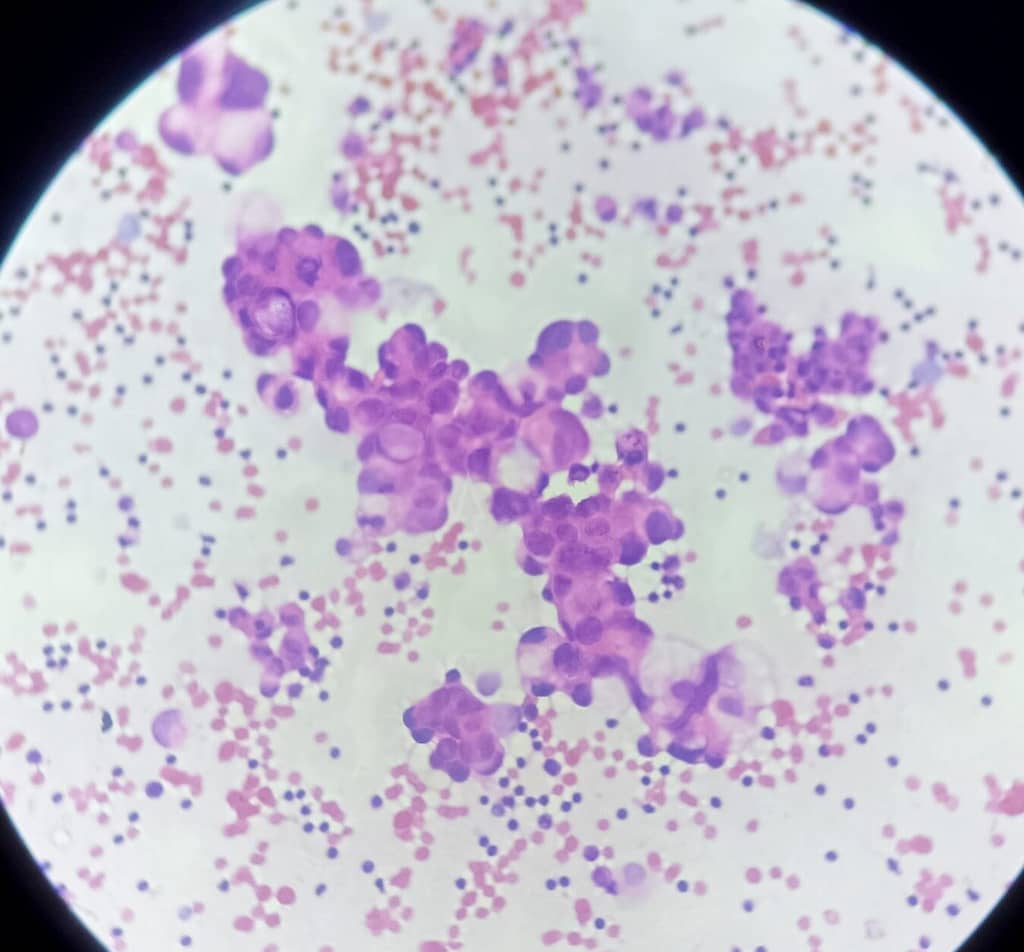
Cytology
In malignant effusions: Atypical cell with high N:C ratio, irregular nuclear
membrane with prominent nucleolus if present are correlated
cytologically for further confirmation of malignancy.
As far as cytological examinations are concerned, it has been demonstrated that cellular integrity is well preserved for up to 48h with appropriate refrigeration(2-8ºC)
The routine cytopathological examination of pleural fluid involves the preparation of both cytospin smears and cell blocks. There are various fixation and staining techniques for cytospin smears and cell blocks
prepared from the sediment after centrifugation.
Slides are usually fixed in 95% isopropyl alcohol and stained with the Papanicolaou method, which clearly brings out nuclear details, thus allowing better identification of malignant cells .
Moreover, cell blocks fixed in formalin are stained with haematoxylin and eosin, and represent the ideal specimens for immunohistochemistry. A cytospin material, including previously Pap-stained slides, can also be used for immunocytochemical analysis. , that include epithelial membrane antigen (EMA), carcinoembryonic antigen (CEA), calretinin, and thyroid transcription factor-1 (TTF-1) are especially useful for the differential diagnosis between reactive mesothelial cells, adenocarcinoma, and mesothelioma.
Cell block can used for further molecular analysis or FISH analysis for EGFR mutation ,KRAS mutation ,ALK-1 detection study .
References:
Henry’s Clinical Diagnosis and Management by Laboratory Methods, 23rd Edition by Richard A. McPherson and Matthew R. Pincus
UpToDate: Pleural Fluid Analysis in Adults with a Pleural Effusion
Shital P.Mirza M.Gondhali G. Pleural fluid ‘cell block’ analysis in malignant pleural effusion: sensitive, superior over fluid cytology and suitable for immunohistochemistry analysis (IHC), will decrease need for thoracoscopy guided procedures.Eur Respir J. 2017; 50 (accessed November 4, 2021)https://doi.org/10.1183/1393003.congress-2017.PA4308