Introduction : A reticulocyte count is a laboratory test that measures the number of immature red blood cells, known as reticulocytes, in the bloodstream.
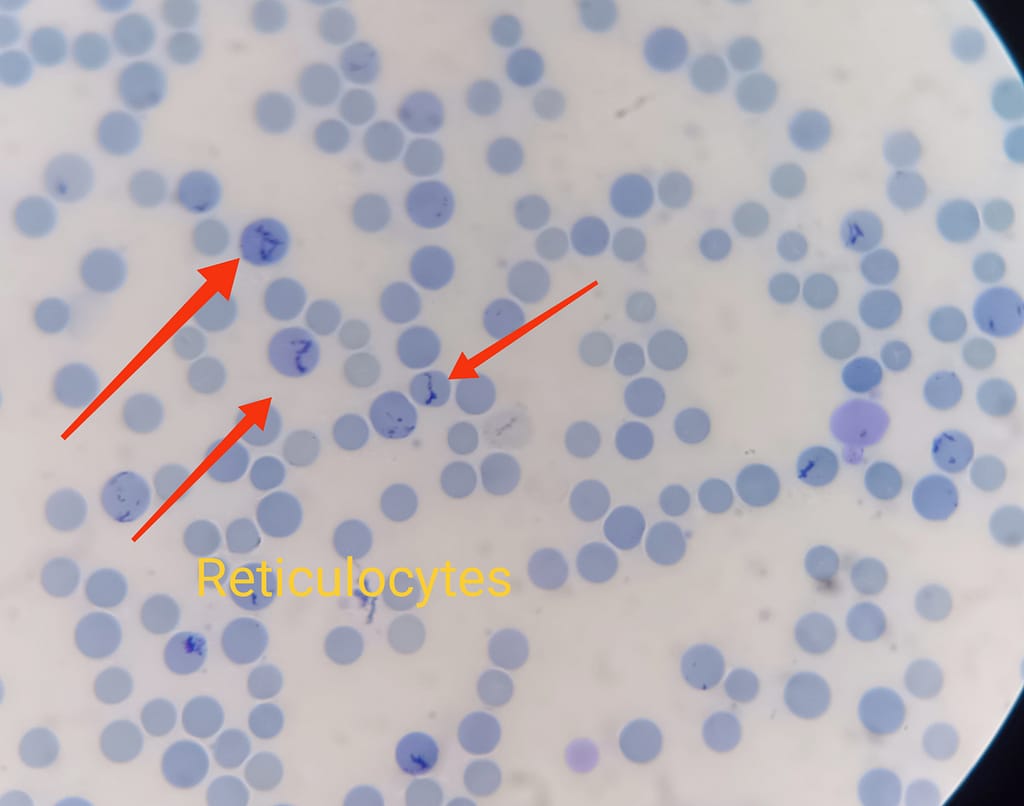
New methylene blue or brilliant cresyl blue (supravital stains) allow visualization of the reticulin network of erythrocyte ribosome in newly formed red blood cells
Why Is Reticulocyte Count Important?
Reticulocyte is particularly useful in evaluating the bone marrow’s ability to produce and release red blood cells into circulation. Reticulocytes are a crucial component of the body’s response to conditions that result in decreased red blood cell levels, such as anemia or blood loss
Also reticulocyte count is an important test for people with anemia. It can help to diagnose the cause of the anemia and to monitor the effectiveness of treatment. A high reticulocyte count can indicate that the anemia is being treated effectively, while a low reticulocyte count can indicate that the treatment is not working or that the anemia is getting worse.
In this article, we will outline the step-by-step procedure for performing a reticulocyte count accurately.
Principle of reticulocyte staining:
RNA within the ribosomes reacts with basic dyes such as azure B, brilliant cresyl blue or New methylene blue to form a blue precipitate. This reaction only occurs in ‘vital’ unfixed preparations
On Romanowsky stains: Reticulocytes appear as polychromatophilic (grey/blue) cells
- Sample collection:
- Put on gloves to maintain a sterile environment.
- Choose an appropriate site for blood collection (commonly the antecubital vein).
- Clean the site with an alcohol swab and allow it to dry.
- Collect the blood into an EDTA tube
Preparation of the blood smear:
- Add 2-3 drops/50 µl of methylene blue stain in a glass test tube then add 2-3 drops/50 µl of the patient’s EDTA whole blood
- Mix well and incubate at 37°C for 30 mins.
- Place a drop of the mixed blood sample on a clean microscope slide.
- Use another slide held at a 30-45 degree angle to spread the blood drop across the slide’s surface.
- Allow the slide to air dry completely and and observe under an oil immersion lens.
- Note: The exact volume of blood to be added to the stain for optimal staining depends upon the red cell count. A larger proportion of anemic blood, and a smaller proportion of polycythaemic blood (high RBC count), should be added than normal blood.
Microscopic Counting of Reticulocytes
Examine the smear first under high power 40 X objective to locate the thin portion of the smear where red cells are evenly distributed and no overlapping is present. Cells must contain at least two blue staining particles or one particle linked to a filamentous thread
Then focus on 100 X oil immersion objective and locate area where there are approximately 100 to 150 RBC’s are present per field.
Examine at least 15 fields having 100 to 150 red cells in each field is simultaneously enumerate the reticulocytes and red cells in each field with the help of hand tally counter.
Calculations
- Calculate the reticulocyte count using the following formula:
Reticulocyte count percentage = (Number of reticulocytes counted ÷ Total number of RBCs) x 100
Here is an example of how to calculate the reticulocyte percentage:
- if you have average 100 RBC in one oil immersion field then after examining 10 fields total 1000 RBC will be examined
- in these 10 oil immersion field you counted 20 reticulocytes.
- The reticulocyte percentage will be calculated as follows:
Reticulocyte percentage = (20 reticulocytes / 1000 red blood cells) x 100% = 2%
In this case, the patient has a normal reticulocyte percentage of 2%.
Corrected reticulocyte count:
The corrected reticulocyte count provides a more accurate assessment of the bone marrow’s ability to produce red blood cells, taking into account the degree of anemia. This value is particularly useful in distinguishing between decreased red blood cell production (as seen in iron deficiency anemia or bone marrow disorders) and increased destruction of red blood cells (as seen in hemolytic anemias).
The formula to calculate the corrected reticulocyte count is as follows:
Corrected Reticulocyte Count (CRC) = Reticulocyte Count (%) x Patient’s Hematocrit / Normal Hematocrit
Example
For example, a patient with anemia has a reticulocyte count of 1% and a hematocrit of 40%. The normal hematocrit for the patient’s age and sex is 45%. The corrected reticulocyte count is calculated as follows:
CRC = (1% x 40%) / 45% = 0.89
In this case, the patient has a corrected reticulocyte count of 0.89. This is a low corrected reticulocyte count, which indicates that the bone marrow is not producing enough red blood cells. This could be a sign of a poor response to treatment.
Reference ranges for reticulocyte count
The reference ranges for the reticulocyte count are as follows:
-
Adult/elderly/child: 0.5-2%
-
Infant: 0.5-3.1%
-
Newborn: 2.5-6.5%
Reticulocytosis: Reticulocytosis is a condition in which the number of reticulocytes in the blood are abnormally high. Higher counts may indicate increased red blood cell production, such as in response to anemia or blood loss .
Conditions causing reticulocytosis
- Hemolytic anemias
- Following hemorrhage
- Following treatment of anemias
- splenectomy
- Treatment with Erythropoeitin
Reticulocytopenia: Reticulocytopenia is a condition in which the number of reticulocytes in the blood are abnormally low. Lower counts may suggest decreased red blood cell production, as seen in certain bone marrow disorders or nutritional deficiencies.
Conditions causing reticulocytopenia are
- Iron deficiency anemia,vitamin B12 deficiency
- Aplastic anemia
- Radiation therapy
-
Decreased erythropoietin level (chronic renal failure)
- Untreated pernicious anemia
- Infiltrating Tumor in bone marrow
- pure red cell aplasia

This manual was very helpful to me for understanding reticulocytes count procedure rather than reading lots of books this information was quite easy to search and simple to understand. Thank you Mam.